In Vitro Fertilization
Before we talk about in vitro fertilization (or otherwise in vitro conception, IVF, FIV) we must understand what infertility is.
What is infertility?
Infertility is defined as the inability of a couple to achieve a pregnancy after 12 months of unprotected sexual intercourse. Infertility is a disease of the reproductive system that disrupts the most basic function of humans: reproduction.
Conception (fertilization) is a complicated process that depends on many factors: the production of a healthy sperm by the male and a healthy oocyte (egg) by the female; the fallopian tubes being permeable allowing the meeting of the sperm with the oocyte; the ability of the sperm to fertilize the oocyte after meeting it; the ability of the fertilized oocyte (embryo) to implant in the female uterus and finally a good quality embryo.
On the other hand, for the pregnancy to go full term (9 months), the embryo must be healthy, the uterus must not be affected by congenital or acquired anomalies (fibroids for example) and the pregnant female must have a hormonal balance as normal as possible. When one of these factors is defective, then we have infertility.
What are the causes of infertility?
Male and female infertility each represent 25% of the cases of infertile couples. In 25% of infertility cases, we are dealing simultaneously with male and female factors. Meanwhile, in 25% of cases, it is not possible to identify a possible cause; these cases are classified as idiopathic (unexplained) infertility.
The most common causes of male infertility include azoospermia (the absence of sperm in ejaculate) and oligospermia (a lower than normal amount of sperm in ejaculate). In some cases, we have the formation of sperm but they are abnormal or die before meeting the oocyte (egg). In other cases, male infertility may be the consequence of a genetic disease such as cystic fibrosis or chromosomal abnormalities.
The most common factor causing female infertility is ovulatory dysfunction. Other factors of female infertility are damage to the fallopian tubes (which can occur due to pelvic infections or endometriosis). Congenital uterine abnormalities (septum, bicornuate uterus, unicornuate uterus, etc.) and fibroids (benign tumors of the uterus) are associated with repeated miscarriages.
How is infertility diagnosed?
As we mentioned above, we are dealing with infertility if a couple does not achieve pregnancy after 12 months of unprotected sex. In this case, these couples should seek a doctor who deals with the treatment of infertility (NB, Not all gynecologists have the necessary experience in this direction and not all deal with infertility).
Searching for the causes starts from evaluating the couple's sexual life (whether they have regular contact or not) to searching for various obligatory analyses or tests for evaluating the individual fertile potential.
The diagnostic analyses and procedures recommended for the woman are as follows:
- Transvaginal ultrasound – to assess the condition of the uterus and ovaries
- Hormonal profile – to evaluate the hormones that influence ovulation.
- Basal body temperature chart – to assess if ovulation has occurred.
- Hysterosalpingography – to evaluate the uterine cavity and the patency of the tubes.
- Laparoscopy – to assess the patency of the tubes and the presence or absence of any pathology that may interest the uterus, ovaries, or tubes from the outside.
The diagnostic analyses and procedures recommended for the man are as follows:
- Manual examination – to verify the presence of testicles in the scrotum.
- Scrotal ultrasound – to evaluate the dimensions and structure of the testicles and to diagnose any varicocele (venous enlargement) which might cause damage to sperm production.
- Hormonal profile – to evaluate the hormones that influence spermatogenesis (sperm production).
- Spermiogram – to assess the concentration, motility, and morphology of the sperm in semen.
How is infertility treated?
The treatment of infertility should only begin after both partners have been investigated. In many non-specialized clinics, treatment is started without fully completing the diagnostic protocol. In a good number of cases, treatment is possible after identifying the factor that may have caused infertility. In these cases, this treatment may be through different medications or through various surgical techniques.
In the first case, we can mention medications that stimulate ovulation in the female partner, improve the hormonal profile, the metabolic profile, while in the male partner improve the quality of the sperm. In cases where fibroids, polyps, or different cysts are found in the female partner, then surgical treatment may be necessary through classical surgery or modern minimally invasive surgery (hysteroscopy or laparoscopy).
When medical and surgical treatment fails, then the couple is recommended for artificial reproduction techniques (ART – Artificial reproductive techniques). These techniques can be directly recommended in cases of fallopian tube blockage (in females) or in the case of oligo-azoospermia (in males). In ART we mention artificial intrauterine insemination (IUI) and in vitro fertilization (IVF).
What is artificial intrauterine insemination (IUI)?
IUI is a complex treatment that starts with the case selection; that is, choosing the couples who truly would have a good chance of achieving a successful pregnancy from this procedure. Initially, we have an ultrasound monitoring of follicular growth (with or without ovulation stimulants). At the moment when the follicle reaches dimensions where it is considered mature, ovulation is triggered through an injection containing HCG.
After this injection, ovulation usually occurs about 36 hours later. It is precisely at this moment that the husband's sperm after processing in the laboratory is injected with the help of delicate catheters inside the uterus. IUI is a much simpler and less expensive technique than IVF.
What is in vitro fertilization (IVF)?
In vitro fertilization is the most major and complex treatment for infertility. It should always be preceded by a preparatory phase which includes the evaluation of the infertile history and treatments of the couple, choosing the right stimulation protocol and the application of different medications or procedures which can further optimize the success chances of in vitro fertilization.
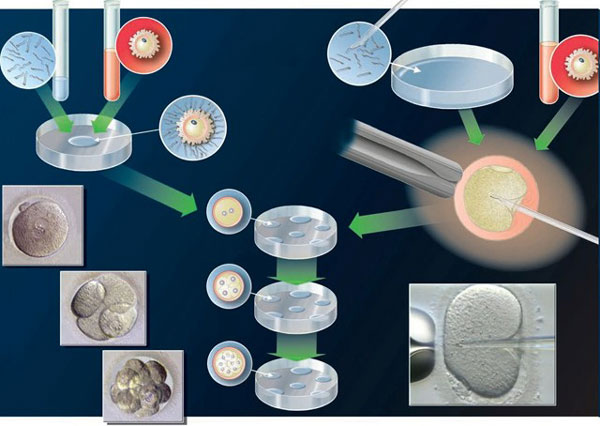
At the beginning of in vitro fertilization, we have the ovarian stimulation phase which lasts about 10 days. Stimulation usually with subcutaneous injections which do not hurt and can be done by the patient herself in an outpatient basis (without the help of a doctor or nurse). During this period, the patient is monitored through transvaginal ultrasound and hormonal dosages to determine as accurately as possible the moment when oocytes (eggs) reach maturity. After the ovarian stimulation phase, the woman undergoes oocyte (egg) aspiration. Aspiration or collection of eggs is done under transvaginal ultrasound guidance and under anesthesia. After this procedure, the patient can leave the hospital within a few hours.
While the oocyte aspiration is happening, the husband provides his sperm in another private room of the clinic. The husband's sperm is examined and from it, the healthiest spermatozoa are selected. In cases of azoospermia (absence of sperm in ejaculate), the patient is recommended surgical sperm extraction from the testicles, a minimally invasive technique that does not last more than 30 minutes.
After collecting the eggs, they are examined by an embryologist and preferably only those with maximum maturity are selected. It is precisely these oocytes (eggs) that are combined with the spermatozoa under the guidance of a microscope. About 40 hours after this combination, fertilization is checked i.e., how many of these eggs have turned into embryos after combining with the spermatozoa. It is precisely this moment (fertilization of the egg) that has given the name to the whole procedure from beginning to end.
Modern clinics now perform micro-manipulation or intracytoplasmic sperm injection (ICSI) which has given hope even to severe cases of male infertility with immobile spermatozoa. During ICSI, the spermatozoon is injected directly under the guidance of an embryologist inside the oocyte (egg). ICSI can and should be performed only by experienced embryologists.
The embryos are kept in the laboratory and transferred into the uterus on days 2, 3, or 5 of their life. The embryo transfer is a painless technique, does not require anesthesia, and is done under ultrasound guidance. The patient can leave the hospital 30 minutes after the transfer. 12 days after the transfer, the patient is advised to perform the beta-HCG analysis which in successful cases will confirm a pregnancy. In cases where many embryos are formed, the couple also has the option of freezing them.
In vitro fertilization has success chances that vary depending on the age of the female partner mainly. Understandably, the older this age, the lesser are also the chances of IVF success. This is explained by the reduction of ovarian reserve especially after the age of 35.
Being more complex, in vitro fertilization is more successful but also more expensive than artificial intrauterine insemination.
Hello!
I am interested to know if the ICSI technique is performed in clinics that perform in vitro fertilization in Albania, and if it is more expensive than the technique of egg fertilization not using intracytoplasmic sperm injection? Thanks
Sent by brandon, më 15 November 2014 në 02:56