Amniocentesis
For prenatal diagnosis, examination of fetal cells is required. This can be achieved through invasive procedures such as amniocentesis or chorionic villus sampling (CVS). Initially, any invasive prenatal diagnosis procedure must be preceded by genetic counseling for the couple, where family genetic history and genetic risk are assessed, and possible complications of the procedure are explained.
Amniocentesis is a technique used for diagnostic (rarely therapeutic) purposes, involving the aspiration of amniotic fluid. It is the most commonly used invasive procedure for prenatal diagnosis. It was first used by Valenti in 1968 for the prenatal diagnosis of Down syndrome. The aspirated amniotic fluid can be analyzed for:
- Karyotype of amniocytes to diagnose chromosomal defects,
- AFP levels to diagnose neural tube defects,
- Lecithin-sphingomyelin ratio to determine fetal lung maturity,
- Bilirubin measurement through spectrophotometric analysis to assess the severity of fetal hemolysis in Rh isoimmunization during pregnancy.
Technique
Traditional amniocentesis is performed after the 15th week of pregnancy. However, amniocentesis can be performed earlier, between the 12th and 14th weeks (early amniocentesis).
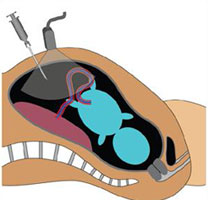
Amniocentesis cannot be understood without an ultrasound examination. Ultrasound is used to determine gestational age, placental location, assess amniotic fluid, and navigate through the spaces it forms, as well as determine the number of fetuses. It should be performed at the same time as amniocentesis.
Every medical procedure strictly adheres to aseptic rules. The abdominal skin is disinfected with a betadine solution. The gloves used are sterile and single-use.
Usually, a spinal needle 22-26 g and 9-14 cm long with a stylet (guide) is used. The needle enters the amniotic cavity under ultrasound guidance. Then, 20-30 ml of amniotic fluid is aspirated and transferred to sterile tubes. These are sent to the laboratory at room temperature.
After the procedure, the mother is shown the fetal heartbeats on the ultrasound monitor. Hospitalization is not necessary. After amniocentesis, the patient can resume normal activities. Strenuous physical effort (beyond normal activity) is not recommended for the 48-78 hours following amniocentesis. The patient should be advised to go to the hospital if she experiences continuous uterine cramps, vaginal bleeding, amniotic fluid leakage, or fever.
Anesthesia?
Usually, local anesthesia is not necessary.
Safety of Amniocentesis
Any procedure involving entry into the pregnant uterus carries a risk to the fetus. Amniocentesis is part of this. Theoretically, it carries a maternal and fetal risk.
Maternal risks are very rare. These may include:
- Chorioamnionitis (in 0.1% of cases).
- Transient vaginal spotting.
- Minimal vaginal leakage of amniotic fluid (in 1% of cases). Usually, this complication is transient.
Fetal risks.
- The abortive risk of amniocentesis is low (< 0.5%).
Indications for Genetic Amniocentesis
- Maternal age at the time of birth >35 years old
- Positive family history for chromosomal anomalies or genetic defects
- Abnormal tests in the second-trimester screening (triple-test).
- Abnormal tests in the first-trimester screening (bi-test).
- Visible anomalies on ultrasound examination.
- Maternal infections potentially harmful to the fetus.
- More than 3 spontaneous abortions.
- High risk for neural tube defects.
- Birth with a history of a fetus with chromosomal defects.
 |
 |
| Figure 1. Schematic presentation of amniocentesis. | Figure 2. Amniocentesis. GA = 16 weeks. |
This article has been summarized from the chapter "Invasive Procedures in Obstetrics" part of the book "Ultrasound in Obstetrical Pathology" published in 2010 by the author.
Hello.
I am pregnant in the 12th week and the gynecologist has recommended that I do amniocentesis in the 16th week of pregnancy.
I wanted to know if it is necessary to do the amniocentesis when all the ultrasounds done so far and all the tests I have taken have turned out normal.
I am 37 years old and this is my second pregnancy. I had two spontaneous abortions before my first pregnancy, in the early weeks of pregnancy, but those were due to carelessness in lifting weights and long travel. I do not have any family history of genetic deformities regarding Down syndrome, quite the contrary. Even my first child was born healthy and without any problems.
Please, I wanted to ask for your advice on whether in my case it is necessary to perform amniocentesis under these conditions, since this technique also carries the risk of miscarriage. A risk not at all desirable for me, who wants to conclude with this pregnancy. Waiting for your response.
With respect,
R. Zeneli
Sent by Rozeta, më 27 Agust 2013 në 02:30
Hello, I have also been suggested to undergo amniocentesis, but apart from the ultrasound, no other tests have been performed on me. When they did the ultrasound, there was a slight swelling on the neck, and I am a bit worried because I know that after the ultrasound, other tests are supposed to be done, and the last option is amniocentesis. I would kindly ask you to explain to me why they have suggested that I directly undergo this serious test
Sent by viola, më 05 October 2013 në 13:45