Gynecological Laparoscopy
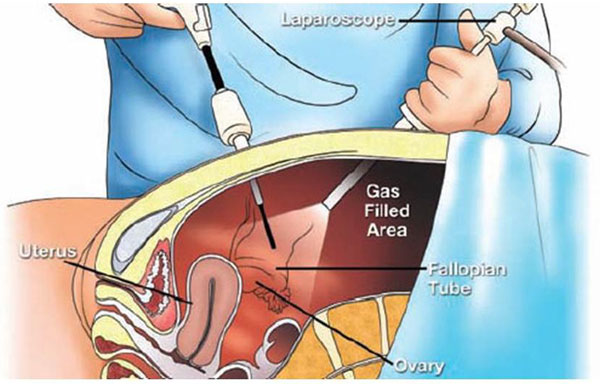
Gynecological laparoscopy is an alternative to open surgery. It uses a laparoscope to look inside your abdomen. On the other hand, open surgery requires an incision (opening) of the abdomen.
The laparoscope is a thin telescope. Through it, the doctor can see inside your abdomen. Gynecological laparoscopy helps us determine if you have endometriosis, uterine fibroids, etc. It also serves to treat such diseases.
Through mini-instruments, the doctor can perform a variety of surgical interventions:
- Removal of ovarian cysts,
- Removal of uterine fibroids (myomas),
- Checking the patency of the fallopian tubes,
- Tubal ligation,
- Hysterectomy (removal of the uterus),
- Etc.
Laparoscopy usually requires a much shorter recovery time than open surgery. Besides, the cosmetic aspect of laparoscopy is absolute as it leaves almost no marks on the skin.
Why should laparoscopy be performed?
Laparoscopy can be used for diagnosis, treatment, or both purposes simultaneously. A laparoscopy can start as diagnostic and end up being therapeutic. Some of the reasons why laparoscopy should be performed are:
- Unexplained pain in the lower abdomen (pelvis),
- Unexplained infertility,
- History of pelvic infection,
What laparoscopy can reveal in these cases includes:
- Endometriosis,
- Uterine fibroids (myomas),
- Cysts or tumors of the ovaries,
- Ectopic pregnancy,
- Pelvic abscess,
- Pelvic adhesions causing chronic pelvic pain,
- Inflammatory pelvic disease,
- Cancer of the reproductive organs (in ovaries, tubes, etc.),
Some of the types of interventions that can be performed through laparoscopy include:
- Removal of ovarian cysts,
- Removal of uterine fibroids Removal of the uterus (hysterectomy),
- Checking the patency of the fallopian tubes
- Removal of the ovaries,
- Treatment of endometriosis (releasing adhesions, removal of endometriotic cysts – endometriomas),
- Tubal plastic surgery (minimally invasive reconstructive surgery aiming at restoring the function of the tubes when possible),
- Various interventions to correct urinary incontinence (Burch Colposuspension),
- Surgical treatment of vaginal vault prolapse after hysterectomy.
How is laparoscopy performed?
Laparoscopy is always performed under general anesthesia. This means you will not feel anything during the procedure. You can resume normal activity immediately 24 hours after the intervention.
While you are asleep, a small tube called a catheter will be inserted into the urinary bladder to collect and control the urine produced during the intervention. Then, through a port inserted at the level of the navel, the abdominal cavity will be inflated with carbon dioxide. The gas will keep the abdominal wall away from your organs as long as the intervention continues. This will reduce the risk of secondary injuries.
After this, through a very small incision at the navel, the operating doctor will pass the laparoscope inside your abdomen. He will transmit the images to a monitor. In this way, the doctor will have a clear view of your organs. Depending on the type of intervention, 2 - 3 additional small incisions < 1 cm may be made, through which other necessary instruments will be passed to manipulate your organs. After completing the intervention, all instruments are removed and the gas is expelled (exhaled). The incisions are closed through stitches (cosmetic adhesive).
Recovery after laparoscopy
After completing the laparoscopy, the recovery and healing time may vary depending on the type of intervention performed. Usually, the time when you can return home varies from a few hours after the procedure to 48 hours after the procedure. In any case, recovery after laparoscopy is much faster than in the case of open surgery.
Mild pain at the level of the navel or back is more than common and insignificant. In some cases, these may also be accompanied by a feeling of nausea. Before leaving the hospital, the doctor will check your health condition and will give you his recommendations regarding any medication or diet for the recovery period.