Knee Prosthesis. (Part Two)
Radiological examination should correlate with clinical signs for knee arthritis. Required radiographs should include a standing antero-posterior (A-P) view, a lateral standing view, and a tangential (skyline view) of the patella. Closure of the joint space, subchondral sclerosis, and osteophytes confirm the diagnosis of osteoarthritis.


The overall mortality rate in Knee Prostheses is less than 1%, but this figure increases with age, in males, and from various past pathologies. Identifying these pathologies before intervention is important for reducing perioperative complications.
An assessment of the patient's social circumstances is important for organizing postoperative rehabilitation.
The examination should also include the assessment of existing scars or soft tissue defects around the knee. Also, a careful assessment of the vascular status of the limb should be made. Systemic or local infections should be identified and treated.
Possible deficits of the quadriceps and extensor mechanisms should be identified and treated through rehabilitation as these can reduce pain and facilitate healing. The range of motion, possible flexion deformities or varus valgus, and records are measured. The best predictor of the range of motion after Knee Prosthesis is the preoperative range of motion.
Indications
The main indication for Knee Prosthesis is the relief of pain caused by severe arthritis. The pain should be significant and disabling. Night pains are particularly indicative. If improper knee function reduces the quality of life, this should be considered. Correction of deformities is an important indication, but rarely used as the primary indication for surgery.
Radiological examination should correlate with the clinical signs for knee arthritis. Patients with lesser loss of joint space, after Knee Prosthesis have less satisfactory results. Exhaustion of all conservative treatments should be considered before surgery.
Knee Prosthesis has an expected lifespan that greatly depends on the level of life activity. Usually, it is indicated for older ages with reduced activity. It is also indicated for younger patients who have limited function as a result of systemic arthritis with involvement of multiple joints.
Young patients in need of a Knee Prosthesis, especially those with post-traumatic arthritis, should not be excluded due to age from prosthetic surgery, but should have a clearly expressed disability in using the knee and be clear about the lifespan of the prosthesis.
Very rarely, severe patello-femoral arthritis may justify prosthesis, as the expected result of prosthesis is superior to patellectomy. Replacement of only the patello-femoral is still under investigation.
Correction of deformities may become the primary indication for prosthesis in patients with moderate arthritis when flexor contracture or varus/valgus laxity is significant. In such cases, usually, more specific prostheses are needed, which brings greater technical difficulties during the intervention as well as more uncertainty in the lifespan of the prosthesis.
Anatomy of the knee
Types of knee movements
Knee movements can be classified as having 6 axes of free movements: 3 translational movements (including antero/posterior, medial/lateral, and inferior/superior) and 3 rotational movements (including flexion/extension, internal/external, and abduction/adduction).
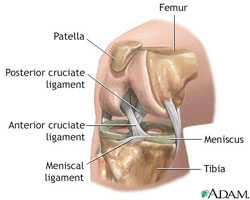
Knee movements are determined by the shape of the articular surface of the tibia and femur, as well as by the orientation of the 4 main ligaments of the knee, which includes the anterior and posterior cruciate ligaments and the medial and lateral collateral ligaments which are connected as a “four-bar linkage system”
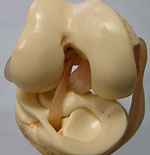
The flexion/extension of the knee involves a combination of rolling and sliding movements called “femoral rollback”, which is a clever way that allows the increase in the range of flexion. Due to the asymmetry between the lateral and medial femoral condyles, the lateral condyle travels a longer distance than the medial condyle during the first 20 degrees of knee flexion. This causes an external rotation of the tibia, which is described as the “screw-home mechanism” of the knee which locks the knee in extension.
The medial and lateral collateral ligament

The primary function of the medial collateral ligament is to counter valgus rotation of the knee, and the secondary function to control the knee's external rotation. The lateral collateral ligament counters varus rotation of the knee and controls internal rotation.
The anterior cruciate ligament
The primary function of the anterior cruciate ligament (ACL) is to resist the anterior displacement of the tibia on the femur when the knee is flexed and to control the “screw-home mechanism” of the tibia in terminal knee extension. The secondary function of the ACL is to resist varus/valgus rotation of the tibia, especially when the collateral ligaments are missing. The ACL also resists the internal rotation of the tibia.
Thank you for the information you provide us. But I have a question. I had a total knee replacement in November 2012 and in December 2014, I slipped on snow and all of my body weight fell on the operated knee (the healthy knee did not touch the ground) the same situation repeated itself also before a month when I slipped again. I am interested to know if these impacts have any negative effect on the lifespan of the prosthesis? Please give me an answer, thank you Ani Terova
Sent by ani terova, më 22 May 2015 në 08:45