Hemostasis and the most common tests for its control (Part One)
Hemostasis is a complex process that is normally activated immediately after damage to the blood vessel (vessels) wall, ensuring the cessation of blood flow (hemorrhage) and subsequently restoring circulation in this vessel (vessels) after the damage is repaired. It involves interactions between blood vessels (structures of the blood vessel walls and endothelial cells lining these vessels from the inside) and blood (platelets and clotting factors).
Normal hemostasis ensures the avoidance of immediate blood loss, a loss that depending on the size and type of vessels (artery, vein, capillary) can range from small amounts (not life-threatening) to large quantities in a short time, risking life as a result of anemia and volume reduction (where in such cases medical and medication help is needed). It develops naturally, unconsciously (meaning we cannot initiate or stop it at will).
The endothelium of the blood vessel is quite smooth, a necessary condition for unobstructed blood circulation. If the endothelium is damaged (atherosclerosis, vasculitis, etc.), that is, its smoothness is compromised, the coagulation process is activated resulting in thrombus formation.
Hemostasis includes:
- Primary hemostasis
- Coagulation
- Fibrinolysis
Primary hemostasis, occurs immediately after damage and consists of: narrowing of the blood vessel lumen (vasoconstriction) and formation of the primary or platelet thrombus.
When the blood vessel is damaged, blood with all its components (cells and plasma) will come out of the vessel wall. The blood vessel, thanks to the elasticity of the wall, narrows and if the vessel's caliber is small, it may lead to the cessation of hemorrhage.
Immediately, platelets will come into action, which will adhere (stick) to the damaged blood vessel wall. The most important factor of adhesion is the von Willebrand factor (vWF), which ensures the connection between the components of the blood vessel wall and the GP-1b receptor, found on the surface of the platelet. The absence of this factor results in von Willebrand disease.
After adhesion, under the action of stimulating factors such as PgI2, Thrombin II will lead to the release of calcium inside the platelets resulting in the activation of the actin-myosin system, consequently changing the shape of the platelet and releasing the contents of platelet granules, where the most important elements are ADP, serotonin, etc.
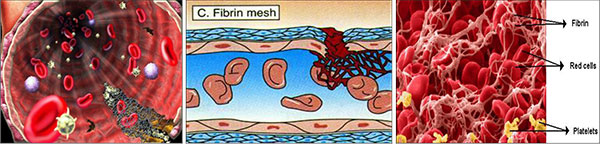
The next stage is aggregation, i.e., the realization of strong platelet-platelet bonds and thereby forming the primary or platelet thrombus, which is soluble, but when the vessel's caliber is small it may stop hemorrhage.
Thus, primary hemostasis consists of the interaction of the blood vessel with platelets and includes platelet adhesion, their shape change, secretion of platelet granule contents, and platelet aggregation leading to the formation of a primary or platelet thrombus.
To evaluate this phase, these tests are used:
- Bleeding time, (BT). It is the time needed to form a platelet thrombus. Bleeding time evaluates the quality, number of platelets as well as the elasticity of the blood vessel wall. More often in practice, Duke's time (the earlobe bleeding time) 1-4’ (on average 3’) is used. The earlobe is pricked and every 30” with an absorbent paper touches (not wipes) the blood drop, until no more blood stain remains on the paper. Before doing BT, the patient should be asked about the medications they are taking. Aspirin should not be taken up to 2 weeks before the test.
- Platelet aggregation is done with an aggregometer.
- Platelet count and evaluation of their morphology. Thus, not only the number of platelets is sought (144,000-444,000 mm3), but also their structure and function. This is seen when their evaluation is done in peripheral blood smears taken with anticoagulant and in smears without anticoagulant (the leukocyte formula) where it is observed if the platelets are or are not arranged in groups.
There are different methods for counting platelets, each with its advantages and disadvantages, but counting platelets in well-prepared peripheral blood smears by an experienced doctor is the best assessment of the number of platelets compared to any other method (optical particle counter).
The most important elements in primary hemostasis are; the blood vessel, the number and function of platelets, and vWF (plasma component). If any of these are damaged, for congenital or acquired reasons, primary hemostasis will be impaired, resulting in hemorrhage or thrombosis.
The coagulation phase (secondary hemostasis). After the formation of the primary (platelet) thrombus during primary hemostasis, inactive coagulation proteins (coagulation factors) present in plasma are activated in a cascade, progressively (one after the other) and secondary hemostasis begins, to end 3-6 minutes later with the formation of the hemostatic or final thrombus (the hemostatic clot).
Coagulation factors (proteins or glycoproteins) are in an inactive state under normal conditions (if they were always in an active phase, the consequence is thrombosis or even hemorrhage from their consumption) there are 13. Coagulation factors include high molecular weight kininogen, prekallikrein, plasminogen, protein C. Ca2+ ions are very important in activating coagulation factors.
All coagulation factors without exception are very important. Quantitative or qualitative damage to each of them, congenital or acquired, equals a thrombotic or hemorrhagic disease and in some cases both together as happens in DIC (Disseminated Intravascular Coagulation).
Most of them are synthesized in the liver (note liver diseases) and factors II, VII, IX, X protein C are Vitamin K-dependent (thus activated by Vit.K). All these factors are replaced by giving plasma and some of them by plasma products (such as cryoprecipitate or pure concentrates of different coagulation factors).
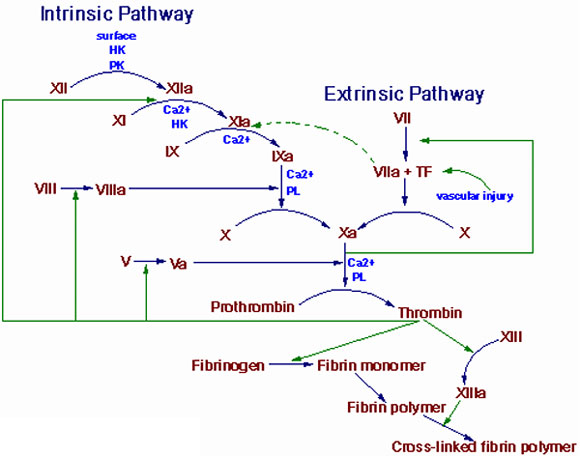
The coagulation phase consists of the external, internal, and common coagulation pathways.
- The intrinsic pathway of coagulation (Intrinsic Pathway) will be activated as a result of damage to the blood vessel wall and exposure of collagen, which through contact (and high molecular weight kininogen) will activate coagulation factor XII which will then activate factors XI, IX, and X (here factor VIII plays an important role).
- The extrinsic pathway of coagulation (Extrinsic Pathway) will be activated as a result of damage to the blood vessel wall and exposure of subendothelial cells to blood, consequently, the tissue factor will be released, which will activate coagulation factor VII that will act directly in activating Factor X.
- So both pathways reach a common point (activation of Factor X) and from here the common coagulation pathway begins with the final consequence of converting fibrinogen to fibrin. Fibrin is placed over the platelet thrombus formed during primary hemostasis. The fibrin network is stabilized by factor XIII and finally, the secondary, hemostatic, or final thrombus is formed, fully fixed at the site of damage and ensuring the cessation of hemorrhage.
Meanwhile, the reconstruction of the damaged blood vessel wall and other surrounding tissues begins.
- The PTT evaluates the coagulation factors XII, XI, IX, VIII, X, V, II (prothrombin), and I (fibrinogen) as well as prekallikrein (PK) and high molecular weight kininogen (HK).
- A PT test evaluates the coagulation factors VII, X, V, II, and I (fibrinogen).
- For coagulation factors, the quantity is assessed with Factor Antigen Assay (for vWF: Ag) and quality, function, activity with Factor Activity Assay (for VWF:RCo or VWF:Act). Initially, Factor Activity is done and then if necessary Factor Antigen (for total and free protein S).
A general information and divided with points and a basic explanation about the topic of Hemostasis (I, II) and laboratory practices...
Sent by Fotaq Veneti, më 29 March 2016 në 18:53
A very valuable information for us medical students. Thank you
Sent by Marsilda Almeta , më 09 January 2020 në 15:53
And I wish you success
Replay from Dr. Shk. Sotiraq Lako, më 11 January 2020 në 12:48
A very valuable information for us medical students. Thank you
Sent by Marsilda Almeta , më 09 January 2020 në 15:53
And I wish you success
Replay from Dr. Shk. Sotiraq Lako, më 11 January 2020 në 12:48