Biliary Atresia(Part One)
Biliary atresia is one of the main causes of cholestatic jaundice in neonates. It is a rare disease of the liver and bile ducts that occurs in newborns. Symptoms of the disease appear about two to eight weeks after birth.
Hepatocytes produce bile which helps in the digestion of fats and also excretes liver products into the intestine.
When the biliary system functions normally, bile drains from the liver into the intestine.
In a neonate with biliary atresia, bile cannot pass from the liver into the intestine, which causes blocking of the bile in the liver leading to damage of the liver cells (cirrhosis) and ultimately liver insufficiency.
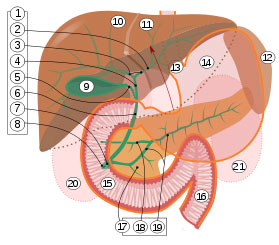
1. Bile ducts
2. Intrahepatic bile ducts
3. Left and right hepatic ducts.
4. Common hepatic duct.
5. Cystic duct.
6. Common bile duct.
7. Ampulla of Vater.
8. Major duodenal papilla.
9. Gallbladder.
10-11. Left and right lobe of the liver.
12. Spleen.
13. Esophagus.
14. Stomach, small intestine.
15. Duodenum.
16. Jejunum
17. Pancreas.
18. Accessory pancreatic duct.
19: Pancreatic duct.
Biliary atresia is not a hereditary disease. The incidence of the disease is 1 in 10,000 children and is more common in girls than in boys. In twins, it has been observed that the disease occurs in only one child or in one child within the family. Asians and African-Americans are more affected by the disease than Caucasians. There seems to be no connection between the disease and any medication or immunization done before or during pregnancy.
Pathophysiology
The cause of biliary atresia is still unknown. Many theories have been proposed regarding the etiopathogenesis of the disease such as infection by reovirus 3, congenital malformations, congenital infection by CMV, as well as autoimmune theories. Although the etiology of the disease is not well understood, many studies have been conducted on the pathogenesis and proper management of progressive hepatic fibrosis, which is the main problem in patients with biliary atresia.
Since the bile ducts cannot transport bile into the intestine, it remains in the liver and leads to hepatic cirrhosis. There is proliferation of small bile ductules and peribiliary fibroblasts are activated. These “reactive” biliary epithelial cells in cholestasis produce and secrete various cytokines such as CCL-2 or MCP-1, Tumor necrosis factor (TNF), Interleukin-6 (IL-6), TGF-beta, Endothelin (ET), and nitric oxide (NO). Among them, TGF-beta is the most important profibrogenic cytokine found in hepatic fibrosis from chronic cholestasis.
During chronic activation of the biliary epithelium and progressive fibrosis, affected patients develop a series of symptoms of portal hypertension such as (bleeding from esophageal varices, splenomegaly, hepatorenal syndrome, hepatopulmonary syndrome).
Two forms of biliary atresia are distinguished: the fetal form that develops during fetal life and is present at the moment of birth, and the perinatal form that is more typical and becomes evident only in the second to fourth week of life.
Doctor, my father suffers from the liver. He has gone through jaundice like his mother, who has now died from this disease. My father has not been treated in the hospital but by the old women. Is this hereditary? Please inform me as I am very worried. Thank you for your understanding
Sent by esmeralda, më 10 May 2014 në 13:55